Blog
About Ketamine
The Ultimate Guide to Ketamine: Types, Properties, and Therapeutic Applications
Introduction: Understanding the Ketamine Renaissance
Ketamine is increasingly recognized as a versatile tool in modern medicine.
Ketamine’s unique properties are making it a focus of ongoing research.
Many practitioners are turning to ketamine for its rapid effects.
Understanding ketamine’s mechanisms is key to its therapeutic applications.
In recent years, ketamine has undergone a remarkable transformation—from a battlefield anesthetic and party drug to a groundbreaking psychiatric and pain management treatment. This versatile molecule is revolutionizing mental healthcare, offering rapid relief to those who have found little help from traditional antidepressants. But what exactly is ketamine, how does it work, and what are the different forms available for therapeutic use?
Recommended products
-
Ketamine Lozenges
Price range: $130.00 through $4,500.00 -
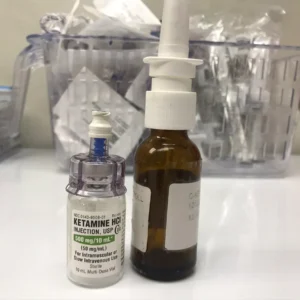
Ketamine Nasal Spray
Price range: $150.00 through $875.00 -
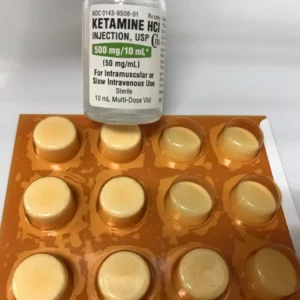
Liquid Ketamine
Price range: $225.00 through $840.00 -
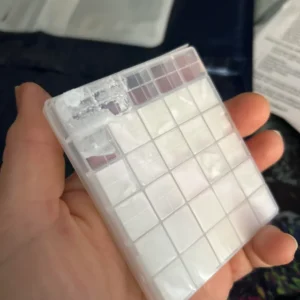
Ketamine Crystal
Price range: $120.00 through $1,050.00 -
Ketamine Powder Ketamine Chemist
Price range: $120.00 through $1,050.00 -
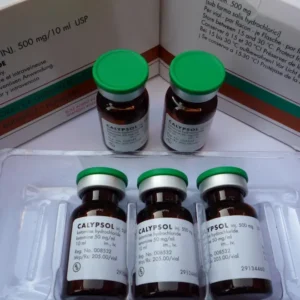
Calypsol Ketamine 50mg/1ml
Price range: $150.00 through $525.00 -
Ketamine Rotex 50mg/1ml
Price range: $150.00 through $525.00 -
Ketamine Tablets
Price range: $130.00 through $500.00 -
Ketamine Shards
Price range: $120.00 through $1,050.00 -
Ketamine Troches
Price range: $145.00 through $4,500.00 -
Ketanir Ketamine 50mg/1ml
Price range: $150.00 through $525.00 -
Ketarol Ketamine 50mg/1ml
Price range: $150.00 through $525.00
Ketamine is paving new paths in psychiatric treatment.
This comprehensive guide explores ketamine’s fascinating journey, its biochemical properties, therapeutic applications, and the critical differences between its various formulations. Whether you’re considering ketamine treatment, researching its potential, or simply curious about this remarkable substance, this article provides a science-based, human-centered exploration of ketamine in all its complexity.
What is Ketamine? A Molecular Perspective
Ketamine, chemically known as (RS)-2-(2-Chlorophenyl)-2-(methylamino)cyclohexanone, was first synthesized in 1962 by Calvin Stevens at Parke-Davis Laboratories. It belongs to the arylcyclohexylamine class of compounds and functions primarily as a non-competitive N-methyl-D-aspartate (NMDA) receptor antagonist.
The Biochemical Mechanism: More Than Just NMDA Blockade
While ketamine’s action on NMDA receptors is its most well-known mechanism, contemporary research reveals a more complex picture:
- NMDA Receptor Antagonism: Ketamine blocks glutamate from binding to NMDA receptors, particularly in the prefrontal cortex.
- AMPA Receptor Upregulation: Secondary to NMDA blockade, ketamine increases glutamate release, which stimulates AMPA receptors, triggering a cascade of neurobiological events.
- BDNF Release: Ketamine stimulates the release of Brain-Derived Neurotrophic Factor (BDNF), promoting synaptic plasticity and growth of new neural connections—a process called synaptogenesis.
- mTOR Pathway Activation: This pathway is crucial for protein synthesis and the formation of new synaptic connections, providing a biological basis for ketamine’s rapid antidepressant effects.
- Opioid System Interaction: Recent research suggests ketamine may also interact with the opioid system, though this remains an area of active investigation.
This multifaceted mechanism explains why ketamine produces effects ranging from anesthesia to profound psychological experiences and rapid antidepressant action.
The Ketamine Family: Different Types and Their Properties
Ketamine exists in two mirror-image molecular forms (enantiomers) and several pharmaceutical formulations, each with distinct properties and applications.
Various formulations of ketamine can cater to different patient needs.
The evolution of ketamine treatment shows promise for many individuals.
Exploring ketamine’s efficacy continues to yield exciting results.
1. Racemic Ketamine: The Original Formulation
Ketamine research is expanding all over the globe.
Chemical Composition: Equal mixture of (R)- and (S)-ketamine enantiomers
Common Formulations: Injectable solution, nasal spray (compounded), troches/lozenges
Racemic ketamine contains both enantiomers in equal proportion and has been the standard form used in medicine since its approval as an anesthetic in 1970. It remains the most widely available and studied form of ketamine.
Therapeutic Properties:
- Anesthetic Effects: Produces dissociative anesthesia characterized by profound analgesia, amnesia, and immobility while maintaining protective reflexes and cardiovascular stability
- Antidepressant Effects: Demonstrated efficacy in treatment-resistant depression at sub-anesthetic doses
- Analgesic Properties: Effective for both acute and chronic pain, particularly neuropathic pain and complex regional pain syndrome
- Psychoactive Effects: Produces dissociation, altered perception of time and space, and potential for mystical-type experiences at higher doses
Pharmacokinetics:
- Onset of Action: 30-60 seconds IV, 2-5 minutes IM, 5-15 minutes intranasal
- Duration: 30-60 minutes IV/IM, variable with other routes
- Metabolism: Primarily hepatic via N-demethylation to norketamine (active metabolite)
- Elimination Half-life: 2-3 hours
2. Esketamine (S-Ketamine): The FDA-Approved Option
Brand Name: Spravato®
Chemical Composition: Pure (S)-ketamine enantiomer
FDA Approval: 2019 for treatment-resistant depression (with oral antidepressant)
Esketamine represents the first FDA-approved ketamine-based treatment for psychiatric conditions. It’s specifically formulated as a nasal spray for administration under medical supervision.
Key Properties and Differences from Racemic Ketamine:
- Potency: Esketamine is approximately twice as potent as racemic ketamine at NMDA receptors due to its 3-4 times greater affinity for the phencyclidine binding site.
- Side Effect Profile:
- Generally causes more dissociation, dizziness, and nausea than racemic ketamine at equivalent NMDA-blocking doses
- May have a more favorable cardiovascular profile with less increase in blood pressure and heart rate
- Clinical Efficacy:
- Demonstrated statistically significant improvement in depression scores in multiple Phase 3 trials
- Particularly effective for acute suicidal ideation
- Requires administration in a certified treatment center with post-dose monitoring
- Administration Protocol:
- Twice weekly for first month
- Weekly for month 2
- Weekly or biweekly thereafter based on response
- Must be taken with an oral antidepressant

3. Arketamine (R-Ketamine): The Promising Newcomer
Current Status: Experimental, not FDA-approved
Chemical Composition: Pure (R)-ketamine enantiomer
While esketamine gained FDA approval, research suggests arketamine may offer some potential advantages, particularly regarding side effects.
Research Findings:
- Antidepressant Efficacy: Preclinical studies show potent antidepressant effects in animal models
- Psychotomimetic Effects: Appears to produce less dissociation and psychotomimetic effects than esketamine at equivalent antidepressant doses
- Neuroplasticity: May have more potent effects on synaptogenesis and BDNF release than esketamine
- Safety Profile: Animal studies suggest less potential for abuse and neurotoxicity
Clinical trials on ketamine demonstrate its rapid antidepressant effects.
Current Status: Arketamine remains in preclinical and early clinical investigation. Its development path suggests potential as a future antidepressant with possibly fewer side effects than esketamine.
Pharmaceutical Formulations: Delivery Methods and Their Properties
Beyond molecular differences, ketamine’s effects vary significantly based on administration route and formulation.
Patients are experiencing significant improvements with ketamine therapy.
1. Intravenous (IV) Ketamine Infusion
Properties:
- Bioavailability: 100% (complete absorption)
- Onset: 30-60 seconds
- Peak Effect: 1-5 minutes
- Duration: 40-60 minutes of acute effects
- Controllability: Highly controllable—infusion can be slowed, paused, or stopped
- Dosing Precision: Most precise method of administration
Clinical Applications:
- Gold standard for treatment-resistant depression in clinical trials
- Chronic pain conditions (CRPS, neuropathic pain)
- Severe, acute suicidal ideation
- Status asthmaticus (off-label)
- Refractory migraine clusters
Advantages:
- Complete bioavailability ensures consistent dosing
- Rapid onset allows for “rescue” in acute psychiatric emergencies
- Titratable—effects can be precisely managed during administration
- Established safety record with anesthesiology monitoring
In some cases, ketamine has shown advantages over traditional treatments.
Disadvantages:
- Requires medical setting with monitoring equipment
- Highest cost among ketamine treatments
- Least accessible for many patients
2. Intramuscular (IM) Injection
Properties:
- Bioavailability: 93%
- Onset: 2-5 minutes
- Peak Effect: 5-20 minutes
- Duration: 60-120 minutes
Clinical Applications:
- Similar to IV but with slightly longer duration
- Sometimes preferred for psychedelic-assisted psychotherapy due to reliable absorption
- Emergency settings where IV access is difficult
Advantages:
- Nearly complete bioavailability
- Simpler administration than IV
- Useful in office-based psychiatric practice
Disadvantages:
- Less controllable than IV—once injected, effects must run their course
- Can be more painful during injection
- Variable absorption in patients with different muscle mass
3. Intranasal Formulations
A. Esketamine (Spravato®):
- Bioavailability: Approximately 45%
- Onset: 5-20 minutes
- Dosing: Fixed-dose device delivering 28 mg per spray
- Administration: Self-administered under direct medical supervision
B. Compounded Racemic Ketamine Nasal Spray:
- Bioavailability: 25-50% (highly variable)
- Customization: Can be compounded in various concentrations
- Use: Often prescribed for at-home use between clinic visits
Advantages of Intranasal Route:
- Non-invasive
- Can be self-administered (with supervision for esketamine)
- Good balance of bioavailability and convenience
Disadvantages:
- Highly variable absorption based on nasal pathology, technique, and formulation
- Nasal irritation common
- Bitter taste from post-nasal drip
4. Oral Formulations (Troches/Lozenges)
Properties:
- Bioavailability: 17-29% (due to extensive first-pass metabolism)
- Onset: 15-30 minutes
- Duration: 60-120+ minutes
- Metabolism: Converted to norketamine (active metabolite) by liver
Types:
- Troches: Hardened lozenges that dissolve slowly in the mouth
- Rapid-Dissolve Tablets: Faster dissolution
- Oral Solutions: Liquid held in mouth
Clinical Applications:
- Maintenance therapy between infusion sessions
- Lower-dose daily regimens for chronic pain
- Patients with needle phobia
- Long-term maintenance treatment
Advantages:
- Convenient for at-home use
- Lower cost than clinic-based treatments
- Norketamine metabolite may contribute to antidepressant effects
Disadvantages:
- Lowest and most variable bioavailability
- Unpleasant taste
- Gastrointestinal side effects more common
- Requires strong patient compliance and proper administration technique
5. Sublingual Formulations
Properties:
- Bioavailability: 25-30%
- Onset: 10-20 minutes
- Absorption: Through oral mucosa, partially bypassing first-pass metabolism
Advantages over Oral:
- Slightly higher bioavailability
- Faster onset than oral
- Less conversion to norketamine
Disadvantages:
- Salivation can reduce effectiveness if patient swallows
- Unpleasant taste
- Mucosal irritation possible
Comparative Analysis: Choosing the Right Formulation
Efficacy Comparison for Depression
| Formulation | Response Rate (TRD) | Time to Onset | Duration of Effect | Maintenance Required |
|---|---|---|---|---|
| IV Infusion | 60-70% | Hours | 7-14 days | Weekly/biweekly |
| IM Injection | 55-65% | Hours | 7-14 days | Weekly/biweekly |
| Esketamine Nasal | 50-60% | 24-48 hours | Variable | Weekly/biweekly |
| Oral/Troche | 40-50% | Days-weeks | Variable | Often daily |
Practical Considerations for Patients
For Rapid Relief of Severe Symptoms: IV or IM administration in a clinical setting provides the most reliable rapid response.
For Long-term Maintenance: Oral or sublingual formulations offer convenience for sustained treatment.
For Those with Needle Phobia: Intranasal or oral routes eliminate needle anxiety.
For Precision Dosing: IV allows the most precise titration to individual response.
For Cost Considerations: Oral formulations are generally most affordable, while IV and esketamine treatments are most expensive.
Therapeutic Applications: Beyond Depression
While depression treatment has dominated recent ketamine research, its applications are remarkably diverse:
1. Psychiatric Conditions
- Treatment-Resistant Depression: The most researched application
- Bipolar Depression: Evidence suggests efficacy without triggering mania at subanesthetic doses
- Post-Traumatic Stress Disorder (PTSD): Reduces symptom severity, particularly when combined with psychotherapy
- Obsessive-Compulsive Disorder (OCD): Emerging evidence for rapid reduction in symptoms
- Suicidal Ideation: Rapid reduction within hours of administration
- Anxiety Disorders: Particularly effective for social anxiety and generalized anxiety
2. Pain Conditions
- Complex Regional Pain Syndrome (CRPS): One of the most effective treatments
- Neuropathic Pain: Diabetic neuropathy, post-herpetic neuralgia, phantom limb pain
- Fibromyalgia: Reduces pain sensitivity and improves function
- Migraine Clusters: Aborts acute attacks and may reduce frequency
- Cancer Pain: Adjunct to opioids for refractory pain
3. Other Medical Applications
- Status Asthmaticus: Life-saving in refractory cases
- Sedation in ICU: Particularly useful in patients with bronchospasm
- Procedural Sedation: Endoscopies, wound care, pediatric procedures
Safety Profile and Risk Management
Common Side Effects by Formulation
All Routes:
- Dissociation/derealization
- Dizziness/lightheadedness
- Nausea/vomiting
- Headache
- Increased blood pressure and heart rate
Route-Specific Side Effects:
- IV/IM: Injection site reactions, more intense dissociation
- Intranasal: Nasal discomfort, bad taste, epistaxis
- Oral: Gastrointestinal upset, dental issues with acidic formulations
- Sublingual: Oral mucosal irritation
Serious Risks and Mitigation Strategies
- Addiction Potential:
- Risk is lower with medical supervision and therapeutic dosing
- History of substance use disorder requires careful screening and monitoring
- Tolerance can develop with frequent use
- Urological Effects:
- High-dose, frequent recreational use associated with ulcerative cystitis
- Therapeutic doses show minimal risk, but monitoring recommended
- Hydration and bladder-protective supplements may be preventive
- Neurotoxicity Concerns:
- Olney’s lesions observed in animal studies at very high doses
- No evidence of similar pathology in humans at therapeutic doses
- Theoretical risk suggests prudent dosing intervals
- Psychiatric Risks:
- Emergence phenomena (unpleasant psychological experiences)
- Potential for worsening symptoms in those with psychotic disorders
- Careful screening and integration support minimizes risks
- Cardiovascular Effects:
- Transient increases in blood pressure and heart rate
- Requires monitoring in those with cardiovascular conditions
- Generally well-tolerated in healthy individuals
The Future of Ketamine Therapeutics
1. Next-Generation Ketamine Derivatives
Researchers are developing ketamine analogs with improved therapeutic profiles:
- Hydroxynorketamine (HNK): Metabolite with antidepressant effects but minimal dissociation
- Deuterated Ketamine: Slower metabolism for longer duration
- Ketamine Esters: Rapidly hydrolyzed for shorter duration when needed
2. Personalized Ketamine Therapy
Emerging approaches include:
- Pharmacogenomic Testing: Identifying responders based on genetic markers
- EEG Biomarkers: Using brain activity patterns to predict response
- Dosing Algorithms: Personalized based on metabolism, weight, and treatment history
3. Integration with Psychotherapy
The combination of ketamine with various psychotherapeutic approaches:
- Ketamine-Assisted Psychotherapy (KAP): Using the altered state for therapeutic work
- Integration Therapy: Processing experiences between sessions
- Protocol-Specific Approaches: Different models for different conditions
4. Expanded Access Models
- Telemedicine Supervision: Remote monitoring for at-home treatments
- Community Clinics: Lower-cost models for wider accessibility
- Insurance Coverage Expansion: Growing acceptance by insurers
Ethical Considerations and Responsible Use
1. Accessibility vs. Safety
The tension between making ketamine available to those in need while maintaining appropriate safety protocols remains a central ethical challenge.
2. Commercialization Concerns
The rapid growth of for-profit ketamine clinics raises questions about:
- Adequate screening and patient selection
- Appropriate medical supervision
- Integration with comprehensive mental healthcare
3. Informed Consent Challenges
Ensuring patients understand:
- The experimental nature of many applications
- Potential risks and side effects
- The importance of integration and ongoing care
4. Regulatory Landscape
- Varied regulations by country and state
- Compounding pharmacy oversight
- Off-label use standards and guidelines
Practical Guide for Those Considering Ketamine Treatment
Step 1: Comprehensive Evaluation
- Medical history review
- Psychiatric assessment
- Screening for contraindications
- Discussion of treatment alternatives
Step 2: Setting Realistic Expectations
- Understanding it’s not a “magic bullet”
- Recognizing the need for ongoing treatment
- Preparing for integration work
Step 3: Choosing a Provider
- Qualifications and experience
- Treatment philosophy and approach
- Safety protocols and monitoring
- Integration support offered
Step 4: Preparing for Treatment
- Medical clearance if needed
- Medication adjustments
- Setting intentions
- Planning integration support
Step 5: The Treatment Experience
- What to expect during administration
- Managing potential side effects
- Creating the right set and setting
Step 6: Integration and Maintenance
- Processing the experience
- Lifestyle modifications to support results
- Determining maintenance schedule
- Ongoing monitoring and adjustment

Conclusion: Ketamine’s Place in Modern Medicine
Ketamine represents one of the most significant psychiatric breakthroughs in decades. Its unique mechanism of action, rapid onset of effects, and efficacy in treatment-resistant conditions have rightfully earned it attention from both the medical community and those seeking relief from debilitating conditions.
The diverse formulations available—from IV infusions to at-home troches—allow for personalized treatment approaches tailored to individual needs, conditions, and circumstances. Each type offers distinct advantages and challenges, requiring careful consideration by both providers and patients.
As research continues to evolve, our understanding of ketamine’s full potential and optimal applications will undoubtedly expand. Current investigations into different enantiomers, metabolites, and administration protocols promise even more refined therapeutic options in the future.
For those considering ketamine treatment, the key lies in:
- Working with experienced, ethical providers
- Understanding the differences between available formulations
- Committing to the full treatment protocol including integration
- Maintaining realistic expectations about outcomes
Ketamine is not a panacea, but for many who have found little relief elsewhere, it offers a promising path toward healing. As we continue to navigate this exciting frontier in mental health and pain management, responsible research, ethical practice, and patient-centered care must remain our guiding principles.
The story of ketamine—from operating rooms to psychedelic therapy clinics—illustrates medicine’s capacity for rediscovery and innovation. As we learn to harness its potential while respecting its power, ketamine may well help rewrite the treatment paradigms for some of our most challenging medical conditions. ketamine as a treatment for depression >> medication what should